PHYSICA PROVIDES AN EXERCISE CLASS BASED ON THE LATEST SCIENTIFIC RESEARCH TO HELP MANAGE OSTEOPOROSIS AND OSTEOPENIA.
Physica Stronger Bones
The Physica Stronger Bones program is a 6-week program of twice-weekly group exercise classes.
You will require an initial assessment prior to starting, so we can assess your needs and design a program that is suitable for you.
Exercise management of osteoporosis must include 3 key components. These are progressive resistance training (strength), impact activities, and balance training.
In addition to the twice-weekly classes, you will also be given a home exercise program. Management of osteoporosis is an ongoing process and regular exercise is a key component.
After the completion of the 5-week program, it is essential you continue with the exercise, especially the impact activities. You may continue this independently, however, you also have the option of moving into one of our Physica Active classes to receive ongoing guidance and progression of your program. These classes are run every day at all our clinics. We offer Physica Active packs (5 or 10 sessions) which are a cost-effective method of participating in a class.
What is Osteoporosis?
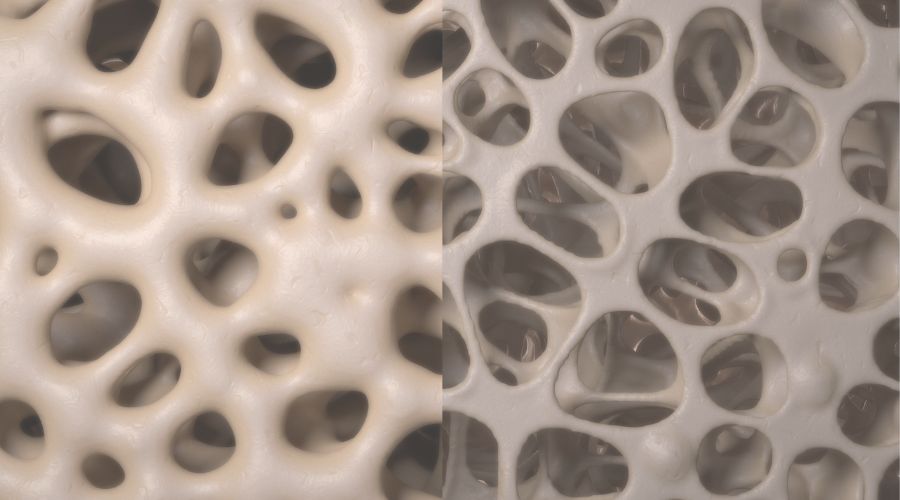
Osteoporosis is a systemic skeletal disorder characterized by compromised bone strength, leading to an increased susceptibility to fractures. This condition results from an imbalance between bone formation and bone resorption processes, leading to a net loss of bone mass and deterioration of bone microarchitecture. Osteoporosis predominantly affects older individuals, particularly postmenopausal women and elderly men, though it can also manifest in younger individuals due to various underlying factors.

Advantages of Osteoporosis Classes:
- Enhanced bone density
- Decrease fracture risk
- Increased reaction time
- Enhanced balance and coordination
- Improved mobility
- Augmented muscle strength
- Enhanced physical fitness
- Reduced risk of falls
- Elevated mood and vitality
- Improved cardiovascular health
Cause of Osteoporosis
Osteoporosis is a condition that weakens bones, making them more fragile and prone to fractures. Several factors can increase the risk of developing osteoporosis:
- Age: As we get older, our bones naturally become less dense and more fragile. This is why osteoporosis is more common in older adults, especially postmenopausal women like yourself.
- Gender: Women are at a higher risk of osteoporosis than men. This is because women have smaller, thinner bones, and the hormonal changes that occur during menopause can lead to bone loss.
- Menopause: The decrease in estrogen levels during menopause accelerates bone loss. Estrogen plays a protective role in maintaining bone density, so its reduction can increase the risk of osteoporosis.
- Family History: If you have a family history of osteoporosis or fractures, your risk may be higher. Genetics can influence bone density and susceptibility to bone-related conditions.
- Low Calcium Intake: Calcium is a key building block for bones. If your diet lacks sufficient calcium, your body might take calcium from your bones, weakening them over time.
- Vitamin D Deficiency: Vitamin D helps your body absorb calcium from your diet. If you don't get enough sunlight or have a diet low in vitamin D, it can impact your bone health.
- Inactive Lifestyle: Regular weight-bearing exercises, like walking or weightlifting, help maintain bone density. Leading a sedentary lifestyle can increase your risk of osteoporosis.
- Smoking: Smoking is detrimental to bone health. It can interfere with the body's ability to absorb calcium and decrease bone-building hormones.
- Excessive Alcohol Consumption: Heavy alcohol intake can interfere with bone formation and increase the risk of fractures.
- Low Body Weight: Having a lower body weight, especially a body mass index (BMI) below 19, can be associated with lower bone density and a higher risk of fractures.
- Certain Medications: Some medications, such as long-term use of corticosteroids (like prednisone), can contribute to bone loss over time.
- Medical Conditions: Certain medical conditions like rheumatoid arthritis, thyroid disorders, and gastrointestinal disorders can affect bone health.
It's important to note that while you can't control factors like age and gender, there are many lifestyle choices you can make to reduce your risk of osteoporosis. Ensuring an adequate intake of calcium and vitamin D through diet or supplements, staying physically active, not smoking, and moderating alcohol consumption can all contribute to maintaining strong and healthy bones as you age.
Understanding Bone Density
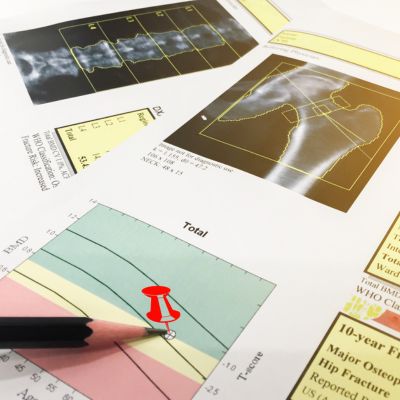
The World Health Organization (WHO) classification for bone density is typically referred to in the context of osteoporosis. The WHO developed a classification system called the "T-score" to assess bone density and categorize individuals into different levels of bone health.
The T-score is calculated by comparing an individual's bone density to the average peak bone density of a young, healthy adult of the same sex. The T-score is used to categorize bone health as follows:
- Normal: A T-score of -1.0 or above indicates normal bone density. This means the individual's bone density is within the expected range for a healthy young adult.
- Osteopenia: A T-score between -1.0 and -2.5 indicates low bone density, also known as osteopenia. People with osteopenia have bone density that is lower than normal but not low enough to be classified as osteoporosis.
- Osteoporosis: A T-score of -2.5 or lower indicates osteoporosis. This means the individual has significantly low bone density and is at a higher risk of fractures.
It's important to note that the WHO classification primarily applies to postmenopausal women and men over the age of 50. For individuals under 50, the Z-score is sometimes used instead of the T-score. The Z-score compares an individual's bone density to the average bone density of individuals of the same age, sex, and ethnic background.
We will calculate your FRAX score and use this to inform building your individualised exercise program.
Bone Fragility Score
The bone fragility scale or score, often referred to as the Fracture Risk Assessment Tool (FRAX), is a clinical tool developed by the World Health Organization (WHO) to estimate an individual's risk of experiencing a major osteoporotic fracture or a hip fracture over a specific period of time (usually 10 years). It takes into account various clinical risk factors and bone mineral density (BMD) measurements (if available) to provide a comprehensive assessment of fracture risk. The FRAX tool calculates the individual's fracture risk based on the input of these factors and provides a numerical estimate of the 10-year probability of major osteoporotic fracture and hip fracture.
Program Outline:
- Initial Assessment: A comprehensive evaluation to understand your unique needs and design a customised program.
- Group Exercise Classes: Engage in twice-weekly group exercise sessions over 6 weeks, facilitated by experienced professionals.
- Home Exercise Program: Receive a tailored home exercise routine to maintain your progress beyond the program.
- Long-Term Benefits: Continue with impact activities to stimulate bone remodeling and mitigate bone loss.
- Physica Active Classes: Transition to ongoing Physica Active classes for sustained guidance and progression.
Take the First Step:
Empower your bone health journey with the Physica Stronger Bones program. Remember, bones respond to loading over time, and our program is designed for sustainable results. Join us in taking charge of your bone health today.
For more information and to enrol in the Physica Stronger Bones program, please visit our website or contact our clinic. Your bones deserve the strength and resilience they were meant to have.
Available at all Physica clinics. Contact our team to find out class times.
